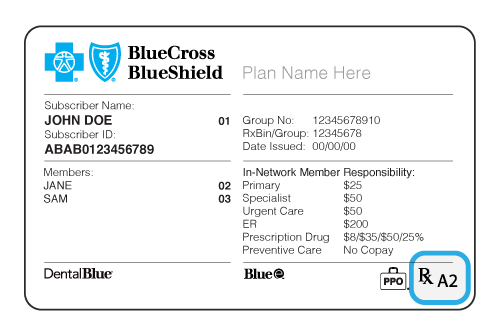
A drug list formulary is a list of generic and brand name drugs covered by a health plan. Xii abbreviation key.
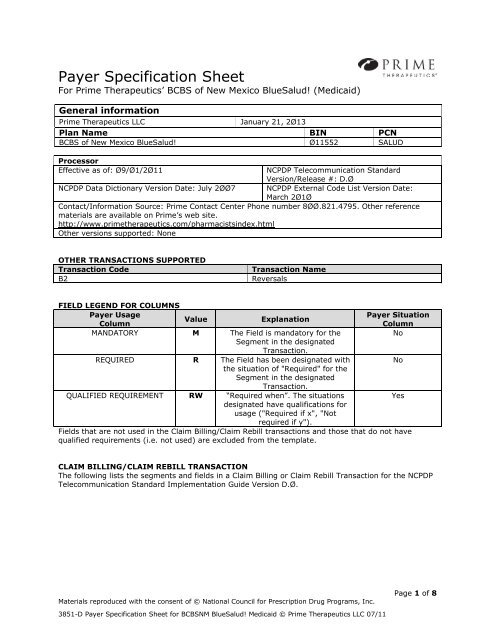
Bcbsnm Medicaid D 0 Pharmacy Payer Sheet Prime Therapeutics
Prime therapeutics tier list. Prime specialty pharmacy a wholly owned subsidiary of prime therapeutics is a leading edge mail order pharmacy built on the strength of smart clinical solutions solid benefit design cost controls and an unwavering commitment to the health and wellbeing of its members. Health insurance marketplace 6 tier drug list august 2020 plan year 2019. Also when adding the new generic drug. The drug list also known as a formulary is regularly updated. You can view the most up to date. Provide cms medicare parts c and d general compliance april 2020 and medicare fraud abuse.
If your employer offers health plan coverage and your prescription drug benefits are administered by prime therapeutics youll find information about prescription drugs when youre signed in. Prime has been a leader on controlled substances misuse for more than a decade. In addition to lists of approved drugs the drug lists also describe how drugs are selected coverage considerations and dispensing limits. Formulary exception formthis document will contain the diagnosis and an explanation for why the prescription is suggested above those which are potentially more commonly used. 5 tier standard drug list please consider talking to your doctor about prescribing preferred medications which may help reduce your out of pocket costs. 2020 formularylist of covered drugs note.
Every pharmacy in primes network must do the following to meet compliance requirements. Prevent detect and report february 2020 training to each pharmacist and pharmacy staff member upon hire and annually thereaftercms training is available on the cms website through their mln. This list may help guide you and your doctor in selecting an appropriate medication for you. If you wish to request coverage for a patients prescription which hasnt been listed on their health insurance providers formulary you will need to fill out a prime therapeutics prior authorization form aka. Replacing it with a new generic drug that will appear on the same or lower cost sharing tier and with the same or fewer restrictions. Bcbsmt uses the prime therapeutics national pharmacy and therapeutics pt committee to review and evaluate new drugs based on safety efficacy and cost.
Blue cross and blue shield of north carolina is an hmo plan with a medicare contract. Our program combines existing and new services to help address this national epidemic. The drug list is developed by a pharmacy and therapeutics pt committee.